Hyperoxaluria: A Hidden Metabolic Threat to Kidney and Systemic Health
Introduction
India is facing a rapidly growing burden of chronic kidney disease (CKD). While lifestyle diseases such as diabetes and hypertension are well-known contributors, rare metabolic disorders also play a significant role. One such underdiagnosed condition is hyperoxaluria, a disorder that is often mistaken for ordinary kidney stone disease, leading to delayed diagnosis and severe complications.
What is Hyperoxaluria?
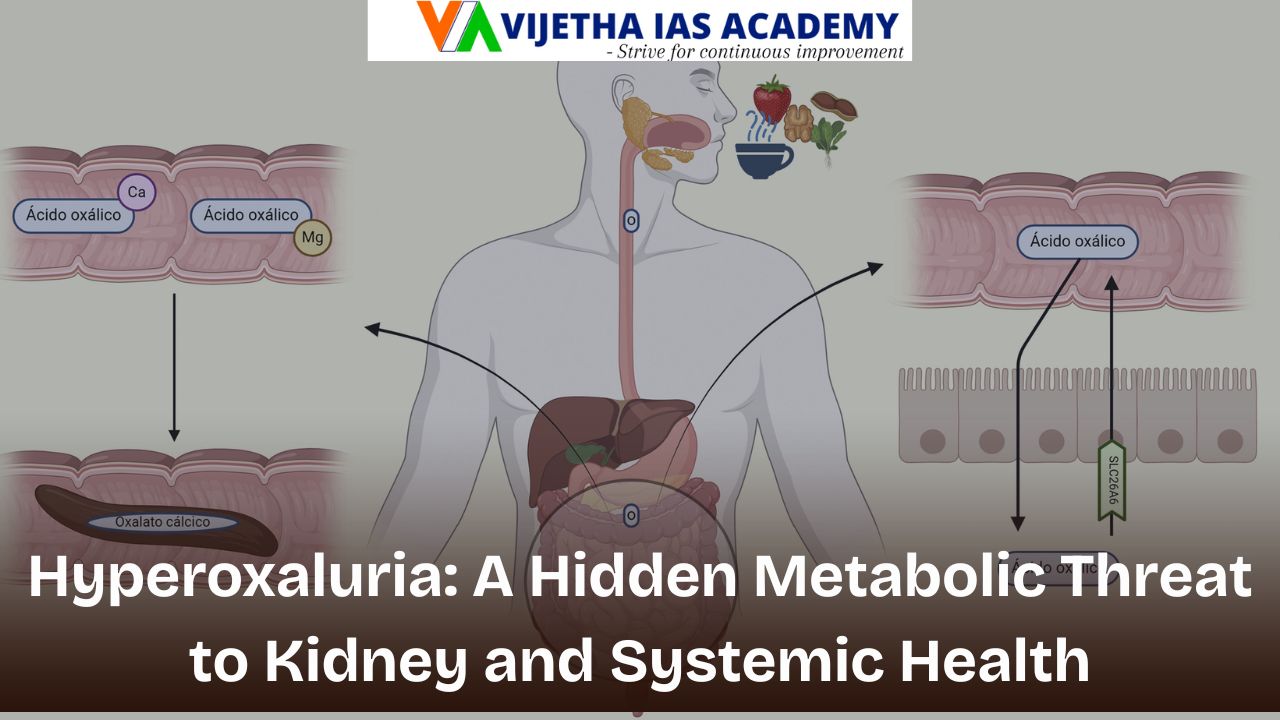
Hyperoxaluria is a metabolic disorder in which the body produces or absorbs excessive amounts of oxalate.
- Oxalate combines with calcium to form crystals.
- These crystals damage kidney tissue over time.
- Progressive damage may lead to kidney failure.
- In advanced stages, oxalate deposits spread to other organs, causing systemic oxalosis.
The disease often progresses silently, making early detection difficult.
Types and Causes
1. Primary Hyperoxaluria
- A genetic disorder caused by defective liver enzymes.
- Leads to continuous oxalate overproduction from childhood.
- Often misdiagnosed as common kidney stones.
2. Secondary Hyperoxaluria
- Caused by increased intestinal absorption of oxalate.
- Associated with:
- Inflammatory bowel disease.
- Fat malabsorption syndromes.
- Post-intestinal or bariatric surgery.
- Aggravated by high-oxalate diets with low calcium intake.
Clinical Manifestations
Early Stage
- Recurrent kidney stones.
- Severe abdominal or back pain.
- Blood in urine.
- Painful or frequent urination.
- Recurrent urinary tract infections.
In Children
- Vomiting.
- Feeding difficulties.
- Poor growth and development.
Advanced Stage: Systemic Oxalosis
When kidney function declines:
- Oxalate accumulates in the blood.
- Deposits occur in multiple organs:
- Bones → fractures and pain.
- Blood vessels → vascular damage.
- Heart → cardiovascular problems.
- Eyes → vision issues.
- Bone marrow → anaemia.
Stakeholders Involved
- Patients and families.
- Primary healthcare providers.
- Nephrologists, geneticists, transplant surgeons.
- Public health system.
- Policy-makers responsible for rare disease frameworks.
Diagnosis and Key Challenges
Major challenges:
- Symptoms resemble common kidney stones.
- Low awareness among doctors and patients.
- Limited access to genetic testing.
- Social stigma and delayed referrals.
Importance of early detection:
- Screening of siblings in affected families.
- Genetic counselling.
- Regular kidney function monitoring.
Treatment and Management
Conservative Measures
- High fluid intake.
- Dietary oxalate restriction (when needed).
- Adequate calcium intake.
Medical Therapy
- Vitamin B6 for certain genetic types.
- RNA-interference therapies to reduce oxalate production.
Surgical and Interventional Care
- Removal of obstructive kidney stones.
- Dialysis in kidney failure (limited effectiveness).
Definitive Treatment
- Combined liver and kidney transplantation.
- Corrects the metabolic defect and restores kidney function.
Ethical and Public Health Dimensions
Ethical issues:
- Inequitable access to genetic testing.
- High cost of advanced therapies.
- Consent and counselling challenges in paediatric cases.
Public health relevance:
- Need to integrate rare diseases into mainstream policy.
- Importance of preventive nephrology.
- Need for early screening in CKD programmes.
Way Forward
- Increase clinician awareness of rare metabolic diseases.
- Strengthen genetic counselling systems.
- Integrate rare kidney disorders into national health programmes.
- Promote research and affordable therapies.
- Create national registries for rare diseases.
Conclusion
Hyperoxaluria demonstrates how rare metabolic disorders can silently evolve into major public health challenges. Early diagnosis, genetic counselling, and timely treatment are crucial not only for individual survival but also for achieving equitable and preventive healthcare.
